BRIDGEPORT, W.Va. — By the point Eric Tennant was recognized in 2023 with a uncommon most cancers of the bile ducts, the illness had unfold to his bones. He weighed 97 kilos and wasn’t anticipated to outlive a 12 months with stage 4 most cancers.
Two years later, grueling rounds of chemotherapy have slowed the most cancers’s progress, even because it has continued to unfold. However chemotherapy has additionally ravaged Tennant’s physique and his high quality of life.
Just lately, nevertheless, the 58-year-old had motive to hope issues would enhance. Final fall, his spouse, Rebecca, discovered of a comparatively new, noninvasive process referred to as histotripsy, which makes use of focused ultrasound waves to destroy tumors within the liver. The remedy may prolong his life and purchase him extra downtime between rounds of chemotherapy.
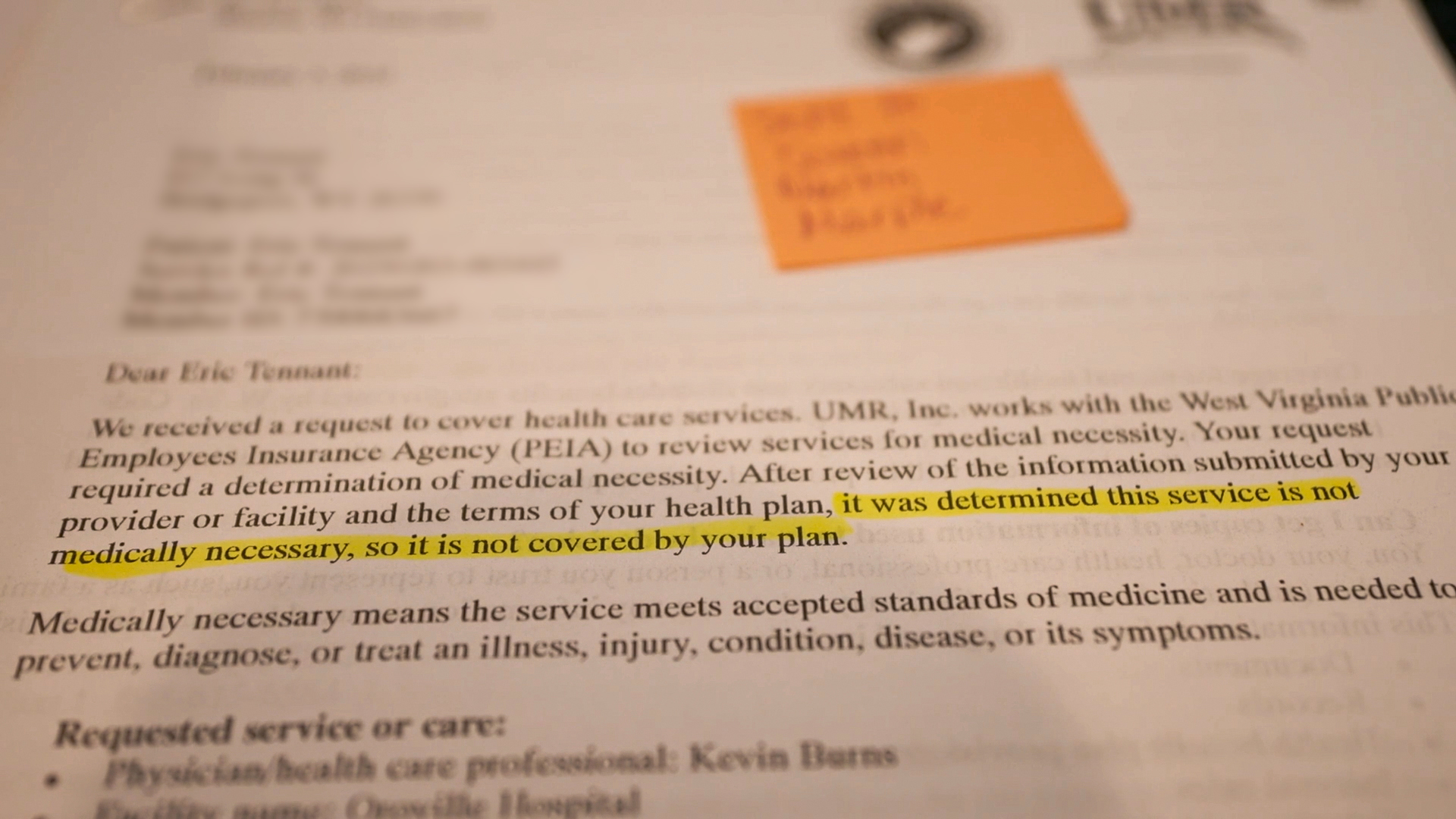
Early this 12 months, Tennant’s oncologist agreed he was a very good candidate for the reason that largest tumor in his physique is in his liver. However that’s when his household started preventing one other adversary: their well being insurer, which determined the remedy was “not medically obligatory,” in response to insurance coverage paperwork.


Well being insurers challenge hundreds of thousands of denials yearly. And just like the Tennants, many sufferers discover themselves caught in a convoluted appeals course of marked by lengthy wait instances, irritating customer support encounters, and selections by medical professionals they’ve by no means met who might lack related coaching.
Latest federal and state efforts, in addition to adjustments undertaken by insurance coverage firms themselves, have tried to enhance a 50-year-old system that disproportionately burdens among the sickest sufferers on the worst instances. And but many docs complain that insurance coverage denials are worse than ever as the usage of prior authorization has ramped up lately, reporting by KFF Well being Information and NBC Information discovered.
When the Tennant household was instructed histotripsy would value $50,000 and insurance coverage wouldn’t cowl it, they appealed the denial 4 instances.
“It’s an enormous mess,” mentioned Rebecca Tennant, who described feeling like a pingpong ball, bouncing between the insurer and numerous well being care firms concerned within the appeals course of.
“There’s actually nothing we are able to do to get them to vary,” she mentioned in an April interview with KFF Well being Information. “They’re, like, not accountable to anybody.”
Whereas the killing of UnitedHealthcare chief government Brian Thompson in December incited a contemporary wave of public fury about denials, there may be nearly no hope of significant change on the horizon, mentioned Jay Pickern, an assistant professor of well being providers administration at Auburn College.
“You’ll assume the homicide of a significant medical health insurance CEO on the streets of New York in broad daylight can be a significant watershed second,” Pickern mentioned. But, as soon as the information cycle died down, “every thing went again to the established order.”
An Unintended Consequence of Well being Reform?
Prior authorization varies by plan however typically requires sufferers or their suppliers to get permission (additionally referred to as precertification, preauthorization, or preapproval) earlier than filling prescriptions, scheduling imaging, surgical procedure, or an inpatient hospital keep, amongst different bills.
The apply isn’t new. Insurers have used prior authorization for many years to restrict fraud, stop affected person hurt, and management prices. In some instances, it’s used to deliberately generate earnings for well being insurers, in response to a 2024 U.S. Senate report. By denying pricey care, firms pay much less for well being care bills whereas nonetheless gathering premiums.
“On the finish of the day, they’re a enterprise they usually exist to earn money,” mentioned Pickern, who wrote concerning the adverse impacts of prior authorization on affected person take care of The American Journal of Managed Care.
For many sufferers, although, the method works seamlessly. Prior authorization principally occurs behind the scenes, nearly at all times electronically, and almost all requests are rapidly, and even immediately, permitted.
However the usage of prior authorization has additionally elevated lately. That’s partly as a result of development of enrollment in Medicare Benefit plans, which rely closely on prior authorization in contrast with unique Medicare. Some well being coverage specialists additionally level to the passage of the Reasonably priced Care Act in 2010, which prohibited well being insurers from denying protection to sufferers with preexisting circumstances, prompting firms to seek out different methods to manage prices.
“However we are able to’t actually show this,” mentioned Kaye Pestaina, director of the Program on Affected person and Shopper Safety at KFF, a well being info nonprofit that features KFF Well being Information. Well being insurers haven’t been traditionally clear about which providers require prior authorization, she mentioned, making it troublesome to attract comparisons earlier than and after the passage of the Reasonably priced Care Act.

In the meantime, many states wish to overhaul the prior authorization course of.
In March, Virginia handed a regulation that may require well being insurers to publicly put up a listing of well being care providers and codes for which prior authorization is required. A North Carolina invoice would require docs who assessment affected person appeals to have practiced drugs in the identical specialty because the affected person’s supplier. The West Virginia Legislature handed payments in each 2019 and 2023 requiring insurers to answer nonurgent authorization requests inside 5 days and extra pressing requests inside two days, amongst different mandates.
And in 2014, the South Carolina Division of Well being and Human Companies quickly lifted all prior authorization necessities for Medicaid beneficiaries in search of rehabilitative behavioral well being providers.
Federal guidelines to change prior authorization that had been launched by the primary Trump administration and finalized by the Biden administration are set to take impact subsequent 12 months, with the intention of streamlining the method, decreasing wait instances, and enhancing transparency.
These adjustments had been supported by AHIP, a commerce group that represents well being insurers.
‘Sick With Little Recourse’
However the brand new federal guidelines received’t stop insurance coverage firms from denying fee for doctor-recommended remedy, they usually apply solely to some classes of medical health insurance, together with Medicare Benefit and Medicaid. Practically half the U.S. inhabitants is roofed by employer-sponsored plans, which stay untouched by the brand new guidelines.
For some sufferers, the stakes couldn’t be greater.
On Could 12, Alexander Schrift, 35, died at dwelling in San Antonio, Florida, lower than two months after his insurance coverage firm refused to cowl the most cancers drug ribociclib. It’s used to deal with breast most cancers however has proven promise in treating the identical sort of mind tumor Schrift was recognized with in 2022, in response to researchers on the Dana-Farber Most cancers Institute in Boston and the Institute of Most cancers Analysis in London.
However Schrift’s insurance coverage firm refused to pay. The Proper to Strive Act, signed by President Donald Trump in 2018, entitles sufferers with terminal diseases to strive experimental medicine, however it doesn’t obligate insurance coverage firms to pay for them.
In Could, Sheldon Ekirch, 30, of Henrico, Virginia, mentioned her dad and mom withdrew cash from their retirement financial savings to pay for remedy denied by her medical health insurance firm.
Ekirch, who was recognized with small fiber neuropathy in 2023, was beneficial by her physician to strive an costly blood plasma remedy referred to as intravenous immunoglobulin to ease her near-constant ache. In April, a state company charged with reviewing insurance coverage denials upheld her insurer’s resolution. Out-of-pocket, the remedy might value her dad and mom tens of hundreds of {dollars}.
“By no means in one million years did I believe I’d find yourself right here,” Ekirch mentioned, “sick with little recourse.”
Earlier this 12 months, New Jersey congressman Jefferson Van Drew, a Republican, launched a invoice that will remove prior authorization altogether. However historical past suggests that will create new issues.
When South Carolina Medicaid lifted prior authorization for rehabilitative behavioral well being providers in 2014, the division’s prices for these providers skyrocketed from $300,000 to $2 million per week, making a $54 million price range shortfall after new suppliers flooded the market. Some suppliers had been ultimately referred to the South Carolina Legal professional Basic’s Workplace for Medicaid fraud investigation. The state Medicaid company ultimately reinstated prior authorization for particular providers, spokesperson Jeff Leieritz mentioned.
What occurred in South Carolina illustrates a typical argument made by insurers: Prior authorization prevents fraud, reduces overspending, and guards in opposition to potential hurt to sufferers.
Then again, many docs and sufferers declare that cost-containment methods, together with prior authorization, do extra hurt than good.

On Feb. 3, 2024, Jeff Corridor of Estero, Florida, grew to become paralyzed from the neck down and spent weeks in a coma after he immediately developed Guillain-Barré Syndrome. The reason for his sickness stays unknown.
Corridor, now 51, argued that the Florida Blue medical health insurance plan he bought on the federal market hindered his restoration by capping the variety of days he was allowed to stay in an acute rehabilitation hospital final 12 months.
Corridor mentioned that after he was pressured to “step down” to a lower-level nursing facility, his well being deteriorated so quickly inside six days that he was despatched to the emergency room, positioned on a ventilator, and required a second tracheostomy. Corridor believes the insurance coverage firm’s protection limits set his restoration again by months — and, satirically, value the insurer extra. His spouse, Julie, estimated Jeff’s medical payments have exceeded $5 million, and most of his care has been coated by his insurer.
“Getting higher will not be at all times the purpose of an insurance coverage firm. It’s a enterprise,” Jeff Corridor mentioned. “They don’t care.”
In a ready assertion, Florida Blue spokesperson Jose Cano mentioned the corporate understands “it may be a problem when a member reaches the restrict of their protection for a selected service or remedy.” He inspired members affected by protection limits to contact their well being care suppliers to “discover service and remedy choices.”
A ‘Uncommon and Distinctive’ Reversal

Again in West Virginia, Eric and Rebecca Tennant say they’re sensible about Eric’s prognosis.
They by no means anticipated histotripsy to remedy his most cancers. At finest, the process may purchase him extra time and would possibly enable him to take an prolonged break from chemotherapy. That makes it value attempting, they mentioned.
As a security teacher with the West Virginia Workplace of Miners’ Well being Security and Coaching, Eric Tennant is a state worker and is insured by West Virginia’s Public Staff Insurance coverage Company.
Because the Tennants pleaded with the state insurance coverage company to cowl histotripsy, they confronted a listing of different firms concerned within the resolution, together with UMR, a UnitedHealthcare subsidiary that contracts with West Virginia to handle the general public worker plans, and MES Peer Overview Companies, a Massachusetts firm that upheld the insurer’s resolution in March, citing that histotripsy is “unproven on this case and isn’t medically obligatory.”
None of their appeals labored. After KFF Well being Information and NBC Information reached out to West Virginia’s Public Staff Insurance coverage Company with questions for this text, the company modified its thoughts, explaining the insurer had consulted with medical specialists to additional consider the case.
“This resolution displays a uncommon and distinctive state of affairs” and doesn’t signify a change within the Public Staff Insurance coverage Company’s general protection insurance policies,” Director Brent Wolfingbarger mentioned in a ready assertion to KFF Well being Information.
In a separate ready assertion, UnitedHealthcare spokesperson Eric Hausman mentioned the corporate sympathizes with “anybody navigating by means of life-threatening care selections.”
“At the moment, there is no such thing as a proof that histotripsy is as efficient as different remedy choices accessible,” he mentioned in late Could, after the sooner insurance coverage denials had been reversed, “and its impression on survival or most cancers recurrence is unknown.”
MES Peer Overview Companies didn’t reply to a request for an interview.
In the meantime, Rebecca Tennant worries it could be too late. She mentioned her husband was first evaluated for histotripsy in February. However his well being has not too long ago taken a flip for the more serious. In late Could and early June, she mentioned, he spent 5 days within the hospital after creating coronary heart and lung problems.

Eric Tennant is not thought-about a viable candidate for histotripsy, his spouse mentioned, though the Tennants are hopeful that may change if his well being improves. Scans scheduled for July will decide whether or not his most cancers has continued to progress. Rebecca Tennant blames her husband’s insurance coverage plan for losing months of their time.
“Time is treasured,” she mentioned. “They know he has stage 4 most cancers, and it’s nearly like they don’t care if he lives or dies.”
Do you might have an expertise with prior authorization you’d prefer to share? Click on right here to inform your story.
NBC Information well being and medical unit producer Jason Kane and correspondent Erin McLaughlin contributed to this report.
